The “Eliminate Health Disparities” strategic direction’s focus is to provide access to comprehensive, quality health care services, which is important for the achievement of health equity and for increasing the quality of a healthy life for everyone. This topic area focuses on four components of access to care: coverage, services, timeliness, and workforce.
Health insurance coverage helps patients get into the health care system. Uninsured people are:
- Less likely to receive medical care
- More likely to die early
- More likely to have poor health status
Lack of adequate coverage makes it difficult for people to get the health care they need and, when they do get care, burdens them with large medical bills. Current policy efforts focus on the provision of insurance coverage as the principal means of ensuring access to health care among the general population. Other factors, described below, may be equally important to removing barriers to access and utilization of services.
Improving health care services depends in part on ensuring that people have a usual and ongoing source of care. People with a usual source of care have better health outcomes and fewer disparities and costs. Having a primary care provider (PCP) as the usual source of care is especially important. PCPs can develop meaningful and sustained relationships with patients and provide integrated services while practicing in the context of family and community. Having a usual PCP is associated with:
- Greater patient trust in the provider
- Good patient-provider communication
- Increased likelihood that patients will receive appropriate care
Improving health care services includes increasing access to and use of evidence-based preventive services. Clinical preventive services are services that:
- Prevent illness by detecting early warning signs or symptoms before they develop into a disease (primary prevention).
- Detect a disease at an earlier, and often more treatable, stage (secondary prevention).
In addition to primary care and preventive services, emergency medical services (EMS) are a crucial link in the chain of care. EMS include basic and advanced life support. Within the last several years, complex problems facing the emergency care system have emerged.17 Ensuring that all persons have access to rapidly responding, pre-hospital EMS is an important goal in improving the health of the population.
Social determinants also play a role; transportation, housing, medical home, translation/ interpreter services, income, geographical location, etc.
Timeliness is the health care system’s ability to provide health care quickly after a need is recognized.
PCPs play an important role in the general health of the communities they serve. However, there has been a decrease in the number of medical students interested in working in primary care. To improve the Nation’s heath, it is important to increase and track the number of practicing PCPs.
The 2020 well-being measures (and objectives) for “Eliminate Health Disparities” are listed below.
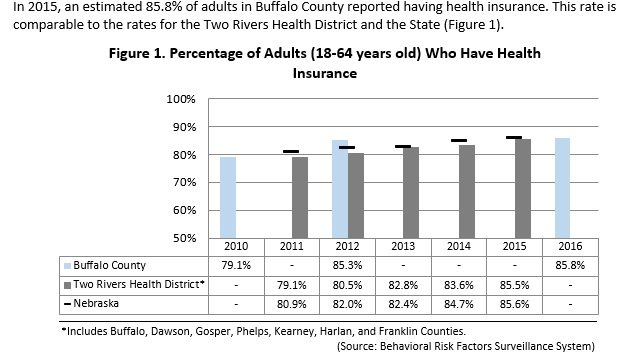
Increase the number adults and children with health insurance
Increase the number of adults reporting “healthy days”
Decrease the number of minority residents reporting barriers to healthcare
Decrease the number of adults without a personal doctor or health care provider
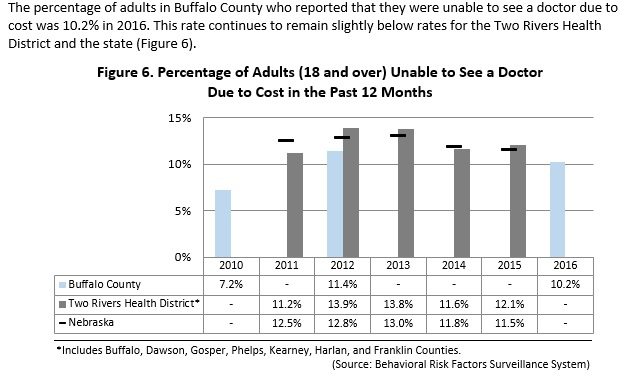
Decrease the number of adults who are unable to see a doctor due to cost
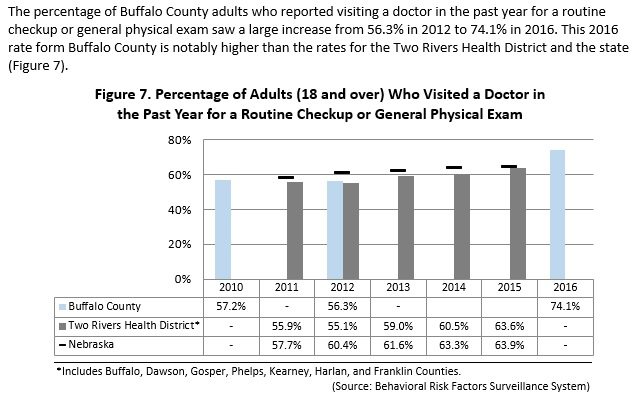
Increase the number of adults who visited a doctor for a routine checkup or physical exam
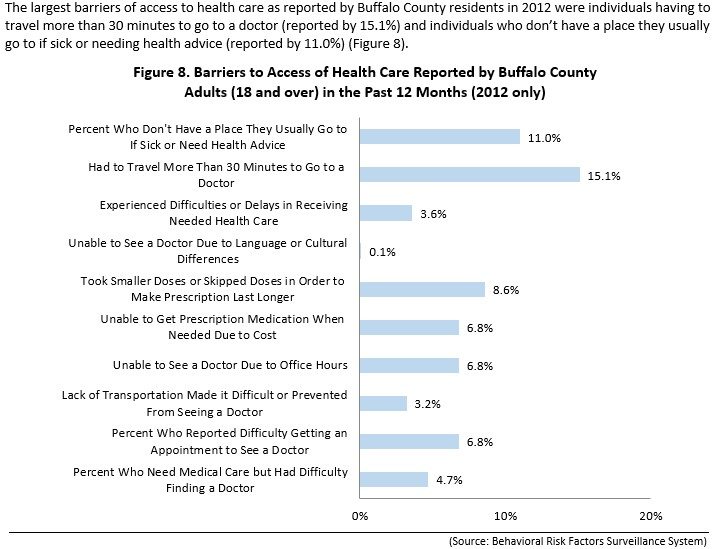
Decrease the number of barriers of access to health care
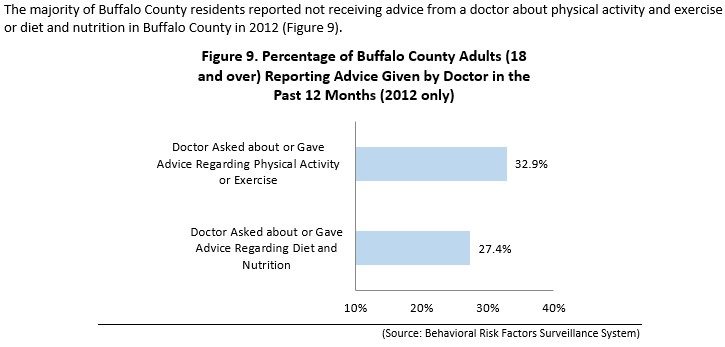
Decrease the number of residents not receiving advice about physical activity, exercise, diet and nutrition
The coalitions that are working toward improving the Active Lifestyle and Healthy Eating well-being indicators: